Integrative Therapeutics For The Age - Related Macular Degenerations
Benjamin Clarence Lane, OD
In 1988, Newsome et al (Arch Ophthalmol 106:192-8)
reported oral zinc may help in the prevention of AMD. In 1984,
Lane had reported interaction of copper and zinc as risk factors
in AMD.
We reviewed for this case-control study, more than 1,000 consecutive nutrition workups of 426 eye patients for whom mineral assays and/or red-blood-cell enzyme concentrations had been determined. Ninety-four of the 426 were confirmed as subject to age-related macular degenerations (AMDs) and identified as cases. The controls were randomly drawn from the remainder after excluding patients with media opacities that prevented adequate photography.
While our evidence supports zinc as a possible, valid risk factor, we find the following
A. Non-exudative ("dry") cases are likely to be deficient in
either zinc and/or zinc's principal antagonist, copper, but excessive
supplementation of either blocks uptake of the other. Odds ratio (OR)
95% confidence interval (CI) = 1.6 to 673.7 as to likelihood of this
deficiency as indexed in hair.
B. Dry “atrophic” AMD cases (characterized by “hard,” discrete,
hydrophilic drusen) are likely deficient in diet-responsive
copper-zinc-dependent superoxide dismutase (SOD) as indexed in red blood
cells, OR = 18 vs age-matched controls [p=0.0027, OR CI=2.5 to
131.3].
C. Active exudative ("wet") AMD cases are 67.5-fold more likely to
present elevated diet-responsive transaminase enzyme titers than
controls, p<0.0001, CI=8.5, 538.3.
D. Excessive well-cooked protein [intake/RDA >1.8] potentiates earlier onset of wet AMD and soft drusen.
E. Even episodic excesses of ascorbic acid intake and elevated
serum lipid-peroxide titers are major risk factors for vitreopathy and
pre-retinal gliosis. Ascorbic acid supplementation ≥ 2,500 mg/day is
associated with increased risk for macular pucker, cellophane
maculopathy, and epi-retinal membranes, OR=9.45, p=0.0004, 95% CI=2.5,
35.4.
F. Elevated LDL is strongly associated with wet AMD and especially with Cystoid Macula Edema.
G. Pre-senile and “Age-Related” choroidal degeneration of the
macula, with variously called “pre-wet, amorphous, indistinct-margin,
confluent, hydrophobic soft-drusen” (and in the absence of significant
hard, discrete drusen) are characterized by elevation of (1)
red-blood-cell SOD, (2) red-blood-cell transaminases, (3) urinary
∂-glucaric acid, (4) plasma-linoleic-fatty acid in ratio to
plasma-gamma-linolenic fatty acid, and (5) dietary protein intake; and
by depression of serum vitamin D3 (25,OH) and of dietary intake of food
calcium in ratio to food phosphorus.
The statistics in (A. through G.) are as reported to the
Association for Research in Vision & Ophthalmology and are based on
approximately 50% of the current data base.
CONCLUSION
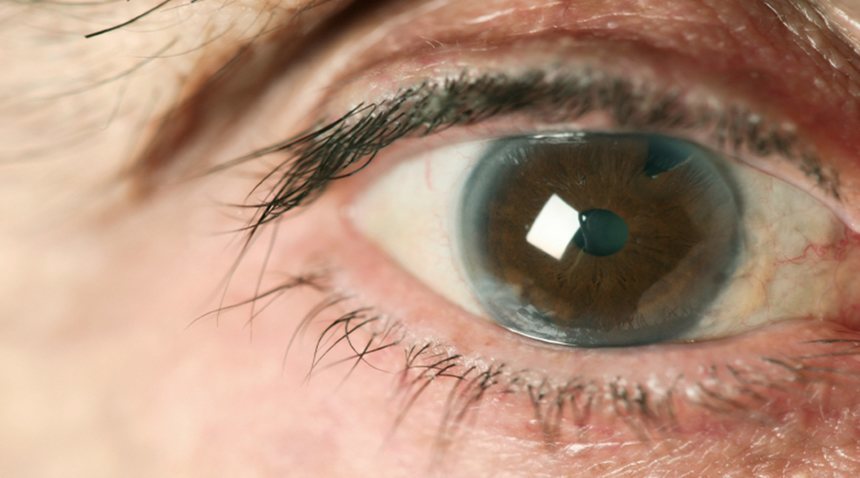
A. Sun exposure, residual ametropia, & SOD and anti-oxidants modulate photo-oxidative insult to pigment-epithelium cells & their phagocytizing functions.
B. Excessive denatured dietary protein and fat create metabolic effects which compromise the blood and the blood-retina barrier.
C. Excessive vitamin C promotes vitreous syneresis, macular pucker, and pre-retinal gliosis
D. Carotenoids, especially including lutein, as best supplied by kale, collard greens, and spinach, so plentiful in the pigment at the macula, have been demonstrated to be vital in protection of the macular area. Supplements containing lutein may became valuable in individuals on aspirin, coumarin, or other blood-thinning therapies and in persons who are not about to eat these green leafy veggies.
Prudent behaviors include avoiding excessive, sustained, unfiltered exposure to bright sunlight, unmonitored supplementation of zinc or copper, excessive protein and fat intake, and excessive ascorbic-acid supplementation, while increasing the intake of fresh, ripe fruits and vegetable salads.
Diet studies and special blood tests can help identify appropriate therapies!
The research need is to differentiate between similar appearing conditions that indeed do have different diagnoses, different mechanisms, and different nomenclature